What is the Reason for a Feeding Tube to Be Inserted in the Nose
Nasogastric (NG) Tube Placement
What is an NG Tube?

Nasogastric (NG) tube
- A nasogastric or NG tube is a plastic tubing device that allows delivery of nutritionally complete feed directly into the stomach; or removal of stomach contents. It is passed via the nose into the oropharynx and upper gastrointestinal tract.
- Note: Other enteral tubing methods involve delivery into the duodenum (nasoduodenal, ND) or jejunum (nasojejunal, NJ) and are used if delivery into the stomach is contraindicated. These are more rare, usually placed by a specialist, and are beyond the scope of this module.
Indications for NG tube:
- Feeding purposes – NICE guidelines state that NG tubes should only be used in people who are malnourished or at risk of malnutrition and have:
- Inadequate or unsafe oral intake, and
- A functional, accessible gastrointestinal tract.
- Examples where both stipulations are met include:
- Neurological conditions causing dysphagia/unsafe swallow such as stroke.
- Lowered consciousness level such as coma or PVS
- Following upper gastrointestinal surgery where a high anastomosis must be protected in the initial post-operative period
- Occasionally, NG feeding is used to prepare malnourished patients for major abdominal surgery in the pre-operative period
- In all cases where enteral tube feeding is considered, specialist assessment by Speech and Language therapists and dieticians is required in order to ascertain that tube feeding is necessary and safe, as well as to monitor the patient's progress once started on enteral feeding in order to determine if and when it can be stopped and how to proceed.
- In general, enteral tube feeding is only advised for up to 4 weeks. After this time, the aim would be for the patient to begin feeding orally, or to change to more long-term measures such as percutaneous endoscopic gastrostomy (PEG).
- If the patient's nutritional needs are not being met or it transpires that the gastrointestinal tract is not functioning normally, Total Parenteral Nutrition (TPN) is considered.
- Medication delivery
- NG tubes can also be used to deliver certain medications directly into the stomach of patients with the same stipulations as feeding.
- Removal of gastric contents
- NG tubes may also be used for removal of gastric contents. Examples would include:
- Initial and continued gastric decompression in the endotracheal intubated patients
- Symptom relief and bowel rest in bowel obstruction (the "drip and suck" conservative management – aspiration of stomach contents in conjunction with intravenous fluid administration)
- Aspirating ingested toxic material
- Diagnostic uses
- Assessment of the presence or volume of upper gastrointestinal bleeding
- Administration ofradiographic contrast
Contraindications for NG tube:
- Absolute contraindications:
- Mid face trauma
- Recent nasal surgery
- Relative contraindications:
- Coagulation abnormalities
- Recent alkaline ingestion (due to risk of oesophageal rupture)
- Oesophageal varices (untreated or recently banded/cauterised)
- Oesophageal strictures
- In the presence of relative contraindications, the advantages and disadvantages of NG placement will have to be judged against the reason for tubing and the patient's condition.
Complications of NG placement:
- Placement may cause:
- Gagging or vomiting
- Tissue trauma along the nasal, oropharyngeal or upper gastrointestinal tract
- Oesophageal perforation (rare)
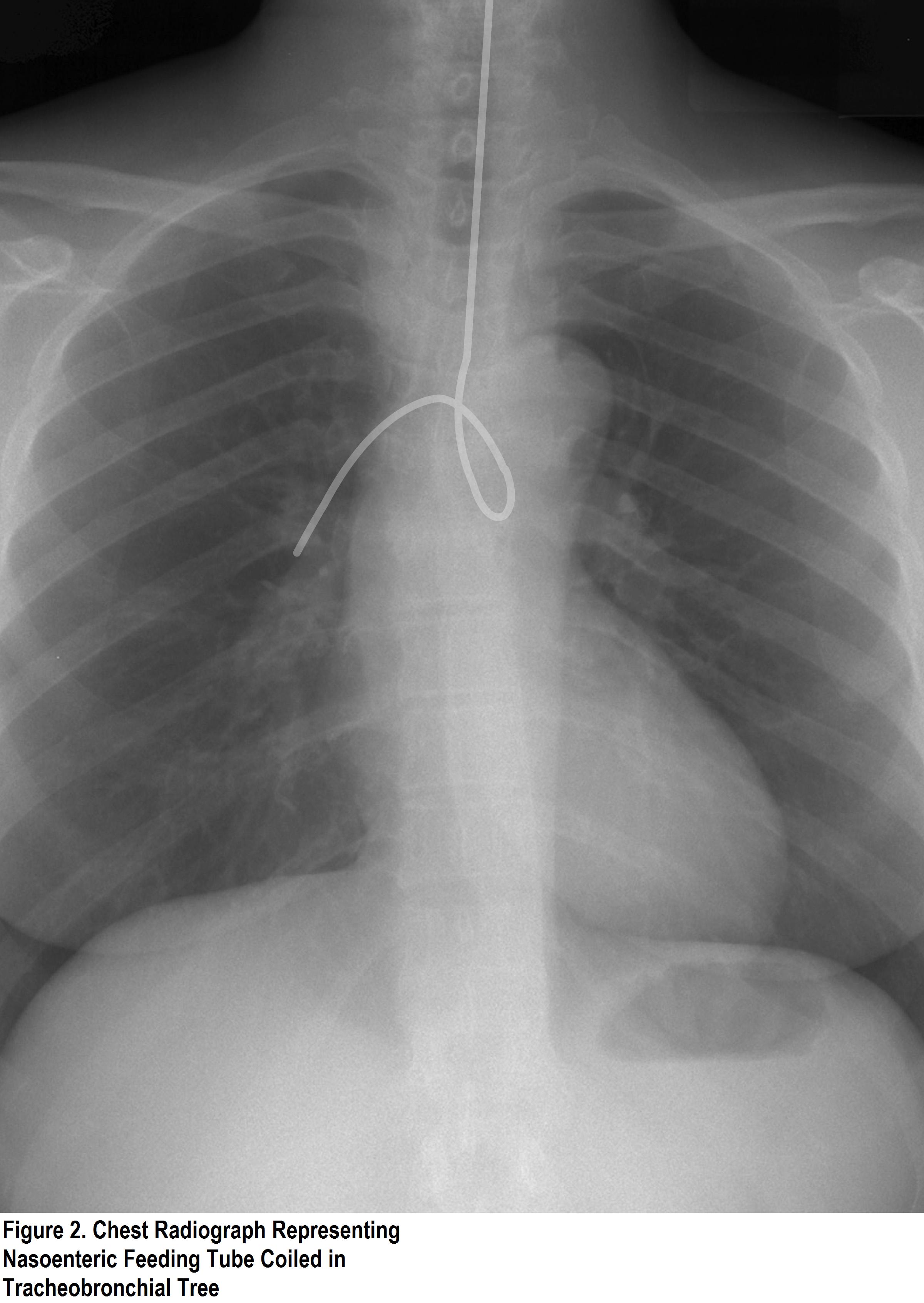
- Incorrect placement leading to respiratory tree intubation may cause aspiration
Equipment needed for placement of NG tubes:
- Nasogastric tube: 16-18 French
- Cup of water with straw
- Tape
- pH indicator
- Gloves
- Emesis basin
- Benzocaine spray (optional)
- Water-based lubricant (optional)
- Suction (have on hand in case of vomiting, particularly in patient with reduced consciousness level)
Positioning for placement of an NG tube:
- The patient should be sat upright with the neck slightly flexed (bringing the nasal canals horizontal) and head supported. For head support, pillows for comfort are adequate in the conscious patient; an assistant may be needed for the unconscious patient.

Correct placement of NG tube
Technique for placement of an NG tube:
- Preparation
- Assemble equipment and take to patient's bedside on trolley.
- Discuss the procedure with the patient including the indications, complications and any alternatives, and obtain consent (written if possible).
- Wash hands and don gloves.
- Ensure patient positioned appropriately
- Examine both nostrils for septal deviation.
- The aim is to identify the more patent nostril for insertion. A tip to help with this is to ask the patient to occlude each nostril in turn and listen to them breathing with each nostril.
- You may wish to apply a local anaesthetic spray to the back of the patient's throat for comfort.
- Measure the NG tube
- Place the NG tube in a position running from the bridge of the patient's nose, to the ear lobe and down to the xiphisternum. Note the distance reached along this path on the NG tube (average length for adult is 55-65cm).
- You may wish to mark this point on the tube with tape.
- Lubricate the 2-4cm tip of the NG tube in either water-based lubricant or simply in water.
- Talk to the patient again to check they are comfortable and build trust. Arrange a signal by which they may communicate with you during the placement if he/she would like to stop – perhaps raising their hand. Always take into account the limitations of each patient (for example, stroke-induced paralysis).
- Insertion
- Insert the tube into the more patent nostril, advancing along the base of the nasal canal directly horizontal towards the nasopharynx.
- When resistance is met at the back of the nasal canal (approx 10-20cm), advance the tube gently as it curves downwards to the pharynx. Never force the tube. It can be useful to twist the tube as you do this.
- Ask the patient to take a sip of water (if safe to swallow) as you advance from the back of the nasal canal to help ease the NG tube towards the oesophagus.
- Stop whenever the distance marker is reached on the NG tube or:
- The tube emerges in the oral cavity
- The patient experiences respiratory distress or if unable to speak
- In the event of nasal haemorrhage
- The tube meets significant resistance
- Post-insertion
- Before removing the guide wire, aspirate from the NG tube and check for gastric pH (0-5). If pH confirmed, remove guide wire and tape tube in place.
- If unable to aspirate from the NG tube, do not remove guide wire, tape wire in place.
- Attach drainage bag or spigot (as appropriate) to end of tube and secure for patient's comfort.
- Discard gloves and wash hands.
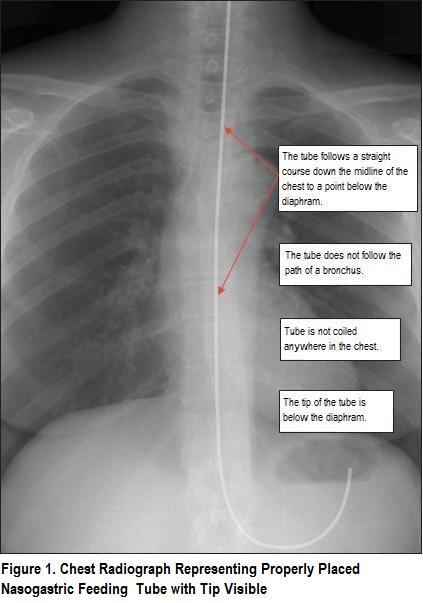
- If unable to confirm placement with pH test, request chest radiograph
- It is important not to start using the tube for feeding purposes until placement is confirmed. Patients on protein pump inhibitor medication or who have undergone previous gastric surgery should always receive a chest radiograph to confirm placement.
- Document consent, size and length of tube inserted, volume and pH of any fluid aspirated, any complications, and whether or not a chest radiograph is required in patient's notes.
How to check an NG tube position on X-Ray:

How to check NG tube position
Management of an NG tube after insertion:
- In the case of NG placement for drainage of stomach contents, the volume and character of the contents should be monitored regularly and documented.
- A standard management protocol is free drainage into bile bag with 4 hourly aspirations.
- In the case of NG placement for feeding, the patient's nutritional and hydration status should be monitored daily, with particular care to monitor electrolytes including potassium, calcium and usually magnesium as well as albumin. This is to aid the dietician in assessing the ongoing needs of the patient and the success or failure of this feeding modality.
- The need for the NG tube should be reassessed regularly and it should be removed as soon as possible, either when symptoms resolve, when clinical decisions render it defunct (for example the decision for operative intervention for bowel obstruction instead of "drip and suck") or after 4 weeks, as per NICE guidelines.
Click here for medical student OSCE and PACES questions about nasogastric (NG) tube placement
Source: https://oxfordmedicaleducation.com/clinical-skills/procedures/nasogastric-ng-tube/


0 Response to "What is the Reason for a Feeding Tube to Be Inserted in the Nose"
Postar um comentário